Unlock 5 Days of Unlimited Access to Our UG Courses - Activate Now
Description: Focuses on the detailed anatomy relevant to surgical practice. It covers the anatomy of various body systems and how knowledge of these structures impacts surgical planning and technique.



150k+ Users Trust Us

2nd Test
MCA Hbti Kanpur“bhvjnkml,;.'/”

NBEMS has introduced time-bound sections in all its MCQ-based examinations which are conducted on computer-based platforms, such as NEET-PG, NEET-MDS, NEET-SS, FMGE, DNB-PDCET, GPAT, DPEE, FDST, and FET, to enhance the exam security and integrity. In this examination pattern, the question paper will be divided into multiple time-bound sections in which each section includes a specific number of questions and allotted time.
In NEET-PG 2024, each of the five time-bound sections (A, B, C, D & E) will have 40 questions and 42 minutes allotted for each section in which candidates cannot proceed to the next section until completing the allotted time for the previous one and can’t review or modify answers afterward.
Candidates have the option to mark questions for review, allowing them to revisit marked questions before the allotted time for that section expires. The number of time-restricted sections may vary based on the total number of questions and operational feasibility in such sections.
These time-bound sections will be implemented in GPAT 2024, NEET-PG 2024, and all upcoming computer-based examination tests conducted by NBEMS, as outlined in respective examination information bulletins.
Stay tuned for more!


Radiology is a study of medical technology, it is a important discipline included in the MBBS typically introduced in the later years of medical training. It covers various imaging techniques used to diagnose and manage diseases, including X-ray, ultrasound, computed tomography, positron emission tomography, nuclear medicine and magnetic resonance imaging.
Radiology serves as a critical link between clinical medicine and diagnostic image technology helping medical professionals to visualize internal structures and identify pathological conditions.
A strong grip in radiology for medical students is important, as it aids in accurate diagnosis, treatment/management planning and monitoring of diseases progression with stages.
The radiology curriculum in MBBS covers topics like principles of imaging modalities, anatomy in imaging, interpretation of radiographs, advanced imaging techniques, radiation safety, and the role of radiology in various clinical scenarios, including trauma, oncology, and pediatric care.
Important Topics in Radiology
In the NEET-PG examination 10- 15 questions are asked, while in the INI-CET there are about 15-20 questions that are based on the Radiology Subject.
These competitive exams mainly cover the extent of the candidates’ knowledge about medical imaging procedures, diagnosis diagnostic accuracy principles and role of radiology in clinical practice.
Acquaintance of subject weightage, typical examination formats, areas of significant potential for high yield and general study strategies can greatly help to improve conceptual understanding of Radiology exam.
Imaging of All Emergencies
- Pneumothorax
- Tension Pneumothorax
- Pneumomediastinum
- Pneumoperitoneum
- Pneumocephalus
- Aortic Dissection
- Aortic Aneurysms and Rupture
- Pseudoaneurysms-Yin yang sign
- Pulmonary Thromboembolism Stroke Imaging-Acute Infarct
- Hyperdense MCA sign
- DWI
- Head Trauma-Epidural hematoma
- Swirl sign
- Subdural hematoma
- Subarachnoid hemorrhage
- Intraparenchymal and intraventricular bleed Abdominal Trauma-FAST
- CECT liver lacerations
- Splenic injury Acute Abdomen-Acute Pancreatitis
- Small and large Intestinal obstruction and Volvulus
X-Rays
Concepts of Kilovolt Peak (KVP) and Milliampere-Seconds (MAS)
- KVP (Kilovolt Peak): Refers to the maximum voltage applied across the X-ray tube, influencing the quality and penetrability of the X-ray beam. Higher KVP results in better image quality with less radiation exposure.
- MAS (Milliampere-Seconds): Indicates the quantity of X-ray exposure, combining the current (mA) and the duration (s) of the exposure. It affects the density and contrast of the image.
Important X-ray Views
- Water View
- Caldwell View
- Rhese View
- Stryker’s View
- Schuller View
- Lordotic View
- Reverse Lordotic View
Radiation Interactions
- Compton Effect
- Photoelectric Effect
- Bremsstrahlung Radiation
Mammography Technique
- Differences from Conventional Radiography
Hysterosalpingography Images
- Normal
- Unicornuate Uterus
- Bicornuate Uterus
- Didelphys Uterus
- Hydrosalpinx
IVP Images
- Ureterocele
- Droopy Lily Sign
- Retrocaval Ureter
CT Scan
Types of CT Imaging
- Spiral CT
- HRCT (High-Resolution CT)
- MDCT (Multidetector CT)
- Dual Energy CT
CT Anatomy
- Brain
- Mediastinum
- Abdomen
- Lungs
Coronary Calcium Scoring
- Agatston Scoring
CT Angiography
- Pulmonary Thromboembolism
Radiation Protection
- Lead Apron
- TLD Badge (Thermoluminescent Dosimeter)
MRI Indications and Contraindications
- MRI Sequences: T1-weighted imaging, T2-weighted imaging, FLAIR (Fluid-Attenuated Inversion Recovery), STIR (Short Tau Inversion Recovery), DWI (Diffusion-Weighted Imaging), DTI (Diffusion Tensor Imaging).
- MR Spectroscopy
- MRI Planes: Axial Images, Coronal Images, Sagittal Images of brain
USG
- Piezoelectric Effect: General of electrical charge in certain materials under mechanical stress
- Ultrasound Phenomena: Posterior Acoustic Shadowing, Posterior Acoustic Enhancement
- FAST (Focused Assessment with Sonography for Trauma
- EFAST (Extended FAST)
- EUS (Endoscopic Ultrasound
- Doppler Ultrasound Techniques: Color Doppler, Spectral Doppler
- Doppler Assessments: Umbilical Artery Doppler, Uterine Artery Doppler, Fetal MCA (Middle Cerebral Artery) Doppler
Radiotherapy
1. Teletherapy
- Linac
- Stereotactic Radiotherapy
- IMRT (Intensity-Modulated Radiation Therapy)
- Craniospinal Irradiation
- Electron Beam
- Proton Beam: Bragg Peak
2. Brachytherapy
- Permanent and Temporary Implants
- Pura Beta Emitters
3. Systemic Radiotherapy
- I-131
- Strontium-89
- P-32
4. Law of Bergonie and Tribondeau
5. Radiosensitivity of Tissues and Tumors
6. Different Iodine Isotopes
- I-131
- I-125
- I-124
- I-123
7. Half-Lives of Important Radioisotopes
- F-18
- Tc-99m
- Iodine Isotopes
- P-32
- Co-60
- Cs-137
Nuclear Medicine
- Thyroid Imaging: Thyroid Scintigraphy, Lingual Thyroid
- Renal Scans: DMSA, DTPA, MAG-3 Scan
- Cardiac Imaging: Myocardial Perfusion Imaging, Myocardial Infarct Imaging
- Bone Imaging
- Sulfur Colloid Scan
- Tc-99m Sestamibi Scan
- Octreotide/Somatostatin Receptor Scintigraphy
- PET Imaging
- HMPAO-SPECT
Neuroradiology
- Imaging of Meningioma
- Tumor Comparisons: Medulloblastoma vs. Ependymoma, Arachnoid Cyst vs. Epidermoid Cyst, Craniopharyngioma vs. Pituitary Adenoma
- Important Named Signs: Mount Fuji Sign, Racing Car Sign, PAND Sign, Hummingbird Sign
- CNS Conditions: TB Meningitis, Creutzfeldt-Jakob Disease (CJD)
- Imaging of Stroke: Hyperdense MCA Sign, Penumbra, CT Perfusion Imaging
- Intracranial Bleeds: Extradural Bleed, Subdural Bleed, Subarachnoid Bleed, Intraventricular Bleed, Intraparenchymal Bleed
Respiratory Radiology
- X-ray Views: Posteroanterior vs. Anteroposterior View
- Medical Conditions: Collapse, Consolidation, Pleural Effusion, Pneumothorax
- Important Signs: Golden S Sign, Luftsichel Sign, Silhouette Sign
- Specific Conditions: X-ray of Pulmonary Edema, Sarcoidosis, Pulmonary Thromboembolism
- CT Imaging: Bronchiectasis, Interstitial Lung Disease, Pulmonary Alveolar Proteinosis
- Fungal and Parasitic Infections: Aspergillosis, Hydatid Disease of the Lung, Lung Abscesses, Fungus Ball, Hydropneumothorax
- Other Findings: Lucent Hemithorax, Foreign Body


DigiNerve is constantly evolving to enhance the user experience while you’re on their journey to becoming a Top Doc. We are excited to bring the latest updates with our commitment to ensure a seamless journey on the go.
Read our monthly newsletter’s September edition (Vol – 2) for the latest updates.
CONTENT UPDATES
PostGrad Course Updates
Dermatology MD:-
1. Chat show on “Scabies and Pediculosis” by Dr. Ragunatha Shivanna, Dr. Priyanka Hemrajani, and Dr. Mariya Babu M. has been added to the course:
Learning Outcomes of the chat show are:
- Understand nature and burden of disease.
- Describe clinical types and clinical features of disease.
- Understand relevance and significance of life cycle of mite and louse in treatment.
- Describe efficacy and safety of therapeutic drugs.
Ophthalmology MD:-
1. Chat show on “Presbyopia Correcting IOLs” by Dr. N. Venkatesh Prajna and Dr. Haripriya Aravind has been added to the course:
Learning Outcomes of the chat show are:
- Indications and contraindications of implanting toric.
- Indications and contraindications of EDOF.
- Indications and contraindications of MFIOLs.
- Factors related to preoperative evaluation, intraoperative pearls and post operative assessment.
Professional Course Updates
Critical Care Simplified:-
1. The panel discussion on “Controversies and Advances in Sepsis” has been added to the module name Sepsis.


Chronic sinusitis is a chronic inflammation of mucous membranes of paranasal sinuses by which irreversible degenerative changes have occurred. Almost invariably succeeds acute sinusitis which did not receive adequate treatment, or it can also develop following a cold or tooth infection.
It occurs when the self-cleansing mechanism of nose and paranasal sinuses gets impaired. Most involved sinusitis is maxillary sinus with duration of symptoms is more than 3 months.
Etiology
Causes of chronic sinusitis are:
- Infection of pharynx, nose and molar teeth
- Trauma to the sinuses and barotraumas
- Local factors include deviated nasal septum, allergy and nasal polypi
- Also includes, chest conditions, such as asthma, chronic bronchiectasis, and chronic bronchitis, responsible for chronic sinusitis.
Chronic sinusitis according to histological changes in the sinus mucosa as follow:
1. Atrophic Sinusitis
Main changes take place in afferent vessels leading to cellular response at and around the arterioles and arteries, later the vessel wall itself becomes thickened and contracted causing endarteritis and thrombosis. In this condition, there is much less edema present as this is primarily a condition that affects the horse’s lower jaw. Hypertrophic and atrophic coexist in the same sinus, the condition causing atrophy at one location and polypoidal hypertrophy at the other place.
2. Hypertrophic Sinusitis
It is characterised mainly by the fact that inflammation is chiefly of the efferent vessels and of the lymphatics. Recurrent stresses take place, which result in changes of the venous and lymphatic flow and organization lead to the formation of oedema and polypoidal mucus membranes, polyps, oedema of periosteum and osteoporosis.
3. Papillary Sinusitis
Occurs when metaplasia of ciliated columnar epithelium to stratified squamous type and throughout the papillary hyperplastic epithelial cells or stroma may be seen inflammatory cells. It is a viral infection.
4. Follicular Sinusitis
Small follicles are seen in the mucous membranes of the sinuses.
5. Glandular Sinusitis
Increase markedly in the submucosal tissue lining of sinuses.
What Kind of Surgery is Done for Chronic Sinusitis?
There are different types of surgery including minimally invasive techniques using endoscopes to remove blockages such as polyps or infected tissue, or to improve drainage in the sinuses. Here are some surgical procedures for chronic sinusitis:
Functional Endoscopic Sinus Surgery
Functional endoscopic surgery is a procedure to re-establish the drainage of the natural ostia and to restore ventilation and mucociliary clearance.
It is based on the principle that clearing the blocked ostium will restore the mucociliary clearance and the diseased mucosa normalizes.
Equipment Used for FESS
- 4 mm 0-degree endoscope
- Angled endoscopes: 30◦, 45◦, 70◦
- Camera
- Display screen
- Light source
Indications for Endoscopic Sinus Surgery
- Chronic Sinusitis
- Nasal Polyps
- Sinus Tumors
- Anatomical Abnormalities
Procedure
- First stack system positioned infront of surgeon. Usually done under general anesthesia, some surgeons prefer local anesthesia especially is unfit patients. Decongestion is done in the observation room with pledgets or nasal patties.
- Patient lies in supine position with head on a ring and head end can be elevated to 15 – 30 degrees.
- The two techniques are:
- Stammberger’s technique (anterior to posterior): Surgery is done from uncinate process towards sphenoid sinus.
- Wigand’s technique (posterior to anterior): Surgery starts from sphenoid sinus and proceeds anteriorly.
- The pledgets/patties soaked in 4% xylocaine adrenaline are removed and a thorough endoscopic examination is done with the three passes.
- First pass, between the septum and inferior turbinate up to choana to visualize the nasopharynx and Eustachian tube.
- In second phase, it passes through middle meatus.
- In third phase, between the superior turbinate and the septum up to the visualization of sphenoid ostia.
- Local infiltration using 2% lignocaine adrenaline given on the axilla of middle turbinate, septum, uncinate process, middle turbinate and lateral wall.
- Uncinate process is identified and the uncinectomy is done.
- Maxillary ostia are identified, widened and the maxillary sinus is cleared.
- Clearance of the anterior ethmoids beginning with the bulla ethmoidalis then done.
- Posterior ethmoids are then cleared after removal of the basal lamella and cleared.
- If there is involvement of the frontal sinus, then the frontal recess is cleared. If there is isolated frontal sinus involvement, it can be accessed without removing the bulls, called as the intact bulla technique.
- Sphenoid sinus can then be approached via the inferomedial aspect of the most posterior ethmoid cell.
- It can also be approached medially by identifying its ostium around 1.5 cm above the roof of the nasopharynx.
- After completion of surgery and achieving hemostasis, nasal packing is done.
Balloon Catheter Sinuplasty (BCS)
Ballon Sinuplasty is a minimally invasive procedure used to treat chronic sinusitis. It includes use o a ballon catheter to dilate the sinus openings, improving drainage and airflow.
Balloon sinuplasty is a medical treatment that is employed by ear, nose, and throat surgeons to open blocked sinus, especially the sinusitis patients who do not respond to drugs.
The United States Food and Drug Administration approved this endoscopic, catheter-based procedure for chronic sinusitis in 2005. It employs the use of a balloon inflated over a wire catheter in order to open up the sinuses passages. It therefore helps to regain normal drainage because when filled the balloon stretches the sinus opening and therefore the walls of the passageway.
Indications:
- Chronic Sinusitis
- Nasal Obstruction
Procedure:
- Patients undergo imaging such as CT scan to assess the sinus anatomy.
- Performed under local anesthesia, sometimes with sedation.
- An endoscope is inserted into nasal passage with small balloon catheter which is threaded into the blocked sinus cavity.
- Balloon is inflated to widen the sinus opening and the balloon is deflated, removed left the passage open.
Frequent Asked Questions (FAQs)
Q1. What are the different types of sinus surgery?
Ans. Here are some different types of sinus surgery:
- Functional endoscopic sinus surgery (FESS)
- Turbinate surgery
- Balloon sinus dilation
- Adenoidectomy
Q2. What is the conservative treatment for chronic sinusitis?
Ans. Chronic sinusitis with polyps should be treated with topical nasal steroids. If severe or unresponsive to therapy after 12 weeks, a short course of oral steroids can be considered. Leukotriene antagonists can be considered.
Q3. What are the differences between Functional Endoscopic Sinus Surgery (FESS) and balloon sinuplasty?
Ans. FESS is a more traditional approach that involves the endoscopic removal of obstructive tissue and polyps to restore sinus drainage. In contrast, balloon sinuplasty is a less invasive technique that utilizes a balloon to dilate the sinus openings without extensive tissue removal. Both techniques aim to improve sinus drainage, but their applications may vary based on the severity and anatomy of the sinus disease.
Q4. What are the potential complications and considerations during the post-operative period for sinus surgery?
Ans. Potential complications include bleeding, infection, and cerebrospinal fluid leaks, although these are relatively rare. Post-operative care involves monitoring for signs of complications, managing pain, and ensuring proper nasal hygiene. Medical students should be aware of the importance of follow-up evaluations to assess healing and address any complications early. Educating patients on signs of complications is also a vital part of post-operative care.

The surgical instrument is a medical device for performing particular actions or achieving desired effects during surgery procedures or operations such as providing access for viewing or modifying biological tissue.
Over time, various surgical instruments and tools have been invented for different surgical procedures. Some common surgical instruments are designed for general use in all kinds of surgeries, while others are designed for specific specialties or medical procedures.
These instruments are essential tools enabling surgeons to access soft tissue, remove bone, dissect and isolate lesions, and treat or eliminate abnormal structures.
Larger/basic medical instruments for surgery are used for the initial exposure, while finer instruments are utilized for navigating delicate structures encountered during procedures.
Surgical Instruments List is Classified According to their Functional Use into the Various Categories
1. Cutting and Dissecting Instruments
These types of surgical instruments are used for cutting skin, dissecting tissues, soft tissues, and even bones through anatomical planes.
2. Grasping and Handling Instruments
Surgeons use these instruments to grasp or hold delicate tissues to help a closer view of their surgical field, one of the most common instruments used for this purpose is forceps including tissue forceps.
3. Clamping and Occluding Instruments
These surgical instruments are used for clamping blood vessels or other tough tissue to keep them away from the area during surgical procedures.
4. Retracting and Exposing
Surgeons used retractors to have a better view of the surgical area. It is used to retract heavy tissues while minimizing trauma during the procedure.
5. An Instrument for Improvement Visualization
Special surgical instruments are designed to visualize internal structures that are not visible externally such as speculums, endoscopes, anoscopes, and proctoscopes.
6. Suturing and Stapling Instruments
These instruments help in crafting to bring together the edges of skin or soft tissue nearby.
7. Suctioning and Aspiration Instrument
In surgical and dental settings, the presence of blood and fluids can obscure underlying structures. Surgeons utilize specialized instruments to clear these fluids from the surgical field, such as the Poole abdominal tip for laparotomy, the Frazier tip for brain and orthopedic surgery, and the Yankauer suction tip for oropharyngeal procedures.
8. Dilating and Probing Instruments
Dilating instruments are used to enlarge orifices like urethra or cervical os. These instruments come in various sizes, from small to large, with surgeons typically beginning with smaller sizes and incrementally, are inserted into natural openings such as the urethra, vagina, or common bile ducts to explore these body cavities.
Here Are Some Common Instruments for Surgical Procedures
1. Scalpel Blades
These instruments are used for initial incision and cutting tissue. It consists of a blade and handle. Surgeons refer to these instruments by their blade numbers.
#10 Blade: Used for making large skin incisions, e.g. in laparotomy.
#11 Blade: Used for precise or sharply angled incisions.
#15 Blade: This one is the smaller version of the #10 blade used for finer incisions.
2. Surgical Forceps
Also called grasping forceps, thumb forceps, locking forceps, or pick-ups, are used for grasping objects or tissue. Can be non-toothed at the tip or toothed (serrated).
Tissue Forceps: It is non-toothed forceps used for traction during dissection and fine handling of tissue.

Adson Forceps: These forceps are toothed at the tip and used for handling dense tissue such as skin closure.

Bonney Forceps: These are heavy forceps used for holding thick tissue e.g. fascial closure.

DeBakey Forceps: This is used for atraumatic tissue grasping during dissection.
Russian Forceps: Used for grasping traumatic tissue during dissection.

3. Clamps
Also known as locking forceps, these are some ratcheted instruments used to hold objects or tissue or provide hemostasis. It can be traumatic or atraumatic.
Allis Tissue Forceps: These are straight along the long axis with a gap to accommodate the tissue between. Sharp teeth at the tip which interlock on closing with minimal crushing of tissues. Used to hold thin structures.

Babcock Tissue Forceps: Its non-traumatic type of forceps, fenestrated and curved blades allow a bulky amount of tissue to be held between. Used to hold soft and firm tissues like the appendix, fallopian tube, ureter, etc.

Kocher’s Hemostatic Forceps: It has a single sharp tooth at the tip of one blade and a groove at the tip of the other blade. The blades are conical blunt with transverse serrations on the inner margins.
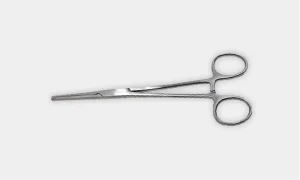
Hemostatic Clamps: Is a non-toothed clamps used in blunt dissection and also used to grasp tissue or vessels that are tied off.

Kelly Clamp: These are the larger size variations of hemostatic instruments with the same function for grasping larger tissues or vessels.

4. Scissors
Used for cutting tissue, suture, or for dissection. Surgical scissors can be curved or straight and used for cutting finer and heavy structures.
Mayo Scissors: These are heavy scissors available in different varieties and also known as suture scissors. Straight scissors are used for suture cutting while curved scissors are used for cutting heavy tissue.

Metzenbaum Scissors: These are lighter scissors used for cutting delicate tissue i.e. heart and for blunt dissection.

Pott’s Scissors: These are fine scissors used for creating precise incisions bein blood and vessels.

Iris Scissors: Used for precise dissection and cutting fine sutures. It serves a multipurpose role for ophthalmic procedures.

5. Needles & Sutures
Needles come in various shapes and cutting edges for different applications. Sutures can be non-absorbable or absorbable and can be available in different sizes.
The shape and curvature of the needle allow use in specialized applications. Straight needles are used for skin and subcuticular suturing while curved needles are used in most general surgical procedures.
There are different types of needles which include:
Conventional Cutting Needle: It is triangular with sharp edges, and one edge faces the inside of the curved needle. This needle is used for tougher tissues such as skin.

Tapered Needle: It is round and tapers to a simple point. It is commonly used in softer tissue such as the intestine but may also be used in tougher tissue such as muscle.

6. Sutures
There are different types of sutures, their classification, and common uses, along with the suture sizes:
| Absorbable | Non-Absorbable | ||
| Braided | Monofilament | Braided | Monofilament |
| Vicryl® Polysorb® | Monocryl® Maxon® PDS® Chromic Gut | Silk | Prolene® Surgipro® Monosof® Nylon |
| Internal Anastomosis | Fascial Closure Subcuticular Skin Closure | Vessel Ligation | Skin Closure Reapproximate Lacerations |
The number associated with surgical sutures denotes the size or diameter of the suture material. Here’s what these numbers typically mean in the context of sutures:
- Lower numbers before the dash (#5, #4) indicate thicker sutures.
- Higher numbers before the dash (#3, #2) indicate thinner sutures.
- More zeros after the dash (#4-0, #3-0) indicate finer sutures.
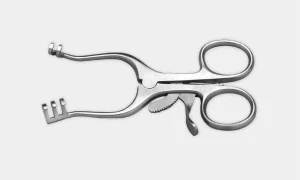
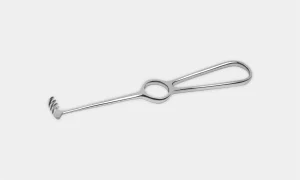
7. Retractors
It varies in different forms, retractor are used to hold an incision open, hold back tissues or other objects to maintain a clear surgical site, or reach other structures. They can either be hand-held or self-retaining retractors via a ratcheting mechanism.
Retractors can be used in various forms in surgery, such as holding incisions open, and retracting tissues or objects to ensure a clear surgical field, or reaching deeper structures. They come in handheld retractor versions or self-retaining types with a ratcheting mechanism for stability.
Deaver Retractor: These are large retractors with broad S-shaped blades. The long handle ends in the form of a hook for better grip. It helps in retracting intra-abdominal cavity viscera like the spleen, and liver during surgeries.

Army-Navy Retractor: It is used to gain exposure to skin layers.

Weitlaner Retractor: Self-retaining retractors for exposing smaller or deep surgical sites. Also known as “Wheaty”.
Richardson Retractor: It can be used to hold back deep tissue structures.

Bookwalter Retractor: Self-retaining retractor system helps in anchoring to the operating table.

Malleable Retractor: Can be customized and bent. Also helps protect the intestines during abdominal closure.

Rake Retractor: Hand-held retractor equipped with sharp teeth used to hold back surface structures.
8. Special Surgical Consideration
Surgical subspecialties typically utilize specialized equipment tailored to their specific procedures. This guide provides a concise introduction to some of these equipments for better familiarity:
Laparoscopic Instruments: These instruments are similar to those used in open surgery, which fit through narrow ports placed through the skin, it work via conducted ports.

Camera & Lens: Camera is a held-hand component, which connects to various lenses. Lenses available with multiple view angles to get better visualization of anatomical structures.

Light Source: It is a fiber optic cable that connects with the lens to illuminate the field of vision.

Insufflator: Used for injecting carbon dioxide into the abdominal cavity which creates space for trocar placement and surgical procedures.

Veress Needle: A technique for creating pneumoperitoneum involves blindly inserting a needle into the abdomen and then injecting gas.

Trocars: Transabdominal ports are used for inserting laparoscopic instruments, as well as for insufflating or extracting specimens. They are available in various sizes such as 5mm, 10mm, and 12mm.

Frequently Asked Questions (FAQs)
Q1. What are some essential instruments for delicate tissue manipulation in microsurgery?
Ans. Instruments used for microsurgery, such as fine forceps for tissue reflection or specialized needle holders like mayo-hear needle holders, are important. These instruments allow precise handling of connective tissue to ensure optimal surgical outcomes.
Q2. How are deep wounds in the abdominal wall managed during surgery?
Ans. Surgical instrumentation for deep wounds includes precise suturing with needle holders, and suction tubes for maintaining a clear field, and these key instruments are designed for delicate tissue manipulation. These tools help surgeons achieve effective closure and enhance surgical outcomes.
Q3. What is the grade of surgical instruments?
Ans. Various types of stainless steels are used to produce surgical instruments; however, there are two main types: 300 series and 400 series. The 400 series stainless steel is hard and used for instruments that require a cutting surface.


Schizophrenia is a serious mental illness that impacts about 1% of the global population. It is characterized by symptoms such as hallucinations, delusions, disorganized speech, and severely disorganized behavior. Additionally, individuals may experience negative symptoms, including diminished emotional expression, lack of motivation (avolition), and cognitive impairments.
Excessive dopamine is found in schizophrenics. Drugs that increase or decrease dopamine are known to worsen or make schizophrenia better.
Schizophrenia Pathophysiology
Schizophrenia’s pathophysiology involves multiple molecular and neural circuit changes, though it’s unclear whether these are direct causes or adaptations to underlying dysfunctions. No current model fully explains all observed changes.
Neurotransmitter imbalances, particularly involving dopamine, serotonin, glutamate, and GABA, are central to schizophrenia. The connection between dopamine and schizophrenia was highlighted by the discovery that D2 receptor blockers can alleviate psychotic symptoms. Four key dopamine pathways—mesolimbic, mesocortical, tuberoinfundibular, and nigrostriatal—play distinct roles. Excessive dopamine in the mesolimbic pathway is linked to positive symptoms, while reduced dopamine in the mesocortical pathway may lead to negative symptoms and cognitive deficits. The nigrostriatal pathway is associated with motor side effects of antipsychotics, and the tuberoinfundibular pathway relates to hyperprolactinemia.
Recent research in cognitive neuroscience has shown that mesostriatal dopamine neurons respond to “reward prediction error,” helping assign significance to stimuli. In schizophrenia, dysregulated firing of these neurons can lead to misattribution of importance to irrelevant stimuli, contributing to delusions and hallucinations.
The relationship between dopamine and schizophrenia is complex, as evidenced by the delay between D2 receptor blockade and clinical response to antipsychotics, suggesting secondary neurochemical mechanisms are also at play. Additionally, the interplay among dopamine, glutamate, and GABA is critical for regulating cortical circuits, with postmortem studies indicating alterations in these microcircuits. This has prompted exploration of targeting glutamate and GABA pathways for improved treatment options.
Stages of Schizophrenia
Phase 1: Initial diagnosis for the earliest signs of schizophrenia.
Phase 2: These are the periods between exacerbations of symptoms, which are relatively calm, but may be deteriorating.
Phase 3: Exacerbation or relapse with increased use of resources.
Major Types of Schizophrenic Disorders
- Disorganized Schizophrenia: Personality is severely disorganized, which includes hallucinations, inappropriate behavior and regression.
- Catatonic Schizophrenia: Acute stupor and sudden loss of animation that alternates with periods of excitement and over activity.
- Paranoid Schizophrenia: Suspicious of everyone and ideas of persecution or grandeur.
- Undifferentiated Schizophrenia: Prominence of psychotic symptoms from more than one subtype or that does not meet the criteria for any subtype.
- Residual Schizophrenia: Absence of prominent psychotic symptoms but continued evidence of symptoms of symptoms such as peculiar behavior and blunted affect.
(Hebephrenic) Disorganized Schizophrenia Type
Individual has facial tics and grimaces, characteristic rises sardonic smile, flat affect with no emotion or strong feeling and in between blunt affect, Volitional affect, and labile affect. Almost all affects are oriented to time place and person.
Pathognomonic are very characteristic:
- Clanging- Rhyming ‘Go to hell, bell’ (pathognomonic).
- Echolalia- Repeating phrase- repeats back “When did you come?”
- Neologisms- Uttering new words without any meaning.
- Pathognomonic are schizophrenics until rules out.
Catatonic Schizophrenia Disorder
Presence of psychomotor retardation, thought process is slow, walking slowly and flexibility is slow. Tendency to talk as though the other person isn’t there! Its tendency is very harmful.
Sometimes rage is combined with anger catatonic excitement and grand blow up can come out with insensitivity to staff.
Increased stress is like increased catatonic excitement.
Paranoid Schizophrenia
The individuals are intelligent with inflated ego (think they are someone special).
Basically, they have severe auditory hallucinations and fear of persecution. They have such fears about safety such as CBI is after them, they being controlled by special messages through electronic media. All delusions start with a kernel of truth.
Undifferentiated Type
The individual has a lot of symptoms. They may have symptoms of all other types so that it is difficult to differentiate.
Kinesics Nonverbal Behaviors
Bizarre behaviors which are outlandish, ridiculous and abnormal but not for drawing attention like shaving of one side of moustache, rose on one side of cheeks, etc.
Symptoms of Schizophrenia
Here are some of the symptoms associated with schizophrenia:
Primary Symptoms of Schizophrenia
- Delusions: False beliefs maintained against logic and contrary evidence.
- Loosening of Associations: Ideas skip from one thought to another in unrelated way.
- Hallucinations: False sensory perceptions in the absence of actual external stimuli.
- Positive Symptoms reflect the presence of unusual behavior and related distortions in form and content of thought.
Secondary Symptoms of Schizophrenia
- Disturbances in affect often blunt or flat.
- Disturbances in volition inability to initiate goal-directed activity.
- Disturbances/interpersonal functioning often withdrawn from others (in the extreme autism).
- Increases psychomotor activity or decreased psychomotor activity.
- Negative symptoms reflect the absence of normally expected behavior.
Diagnosis of Schizophrenia
The diagnosis of schizophrenia relies on two primary systems: the DSM-5-TR and the ICD-10, each with slight variations.
1. DSM-5-TR
The DSM-5-TR, published by the American Psychiatric Association (APA) in 2022, outlines the following criteria for diagnosing schizophrenia:
- Symptom Presence: The patient must exhibit two (or more) of the following symptoms for a significant portion of time during a 1-month period (or less if successfully treated). At least one symptom must be one of the first three:
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior
- Negative symptoms (e.g., diminished emotional expression or avolition)
- Functional Decline: There must be a noticeable decline in functioning in areas such as work or relationships since the onset of symptoms.
- Duration: Continuous signs must persist for at least 6 months, including at least 1 month of active-phase symptoms, which may be shorter if treated. Symptoms can also be prodromal or residual, including negative or attenuated active-phase symptoms.
- Exclusion Criteria: Schizoaffective, depressive, or bipolar disorders with psychotic features must be excluded. Symptoms should not be attributed to substance use, medication, or another medical condition. If a developmental disorder is present, the diagnosis requires at least 1 month of prominent delusions or hallucinations.
2. ICD-10
The ICD-10 specifies that the patient must demonstrate at least one of the following symptoms for a duration of 1 month or more:
- Thought echo, thought insertion or withdrawal, thought broadcasting
- Delusions of control, influence, or passivity; delusional perceptions
- Hallucinatory voices providing a running commentary on the patient or discussing the patient among themselves
- Persistent delusions that are culturally inappropriate or implausible
Alternatively, the patient may exhibit at least two of the following symptoms for 1 month or more:
- Persistent hallucinations in any modality, accompanied by fleeting or half-formed delusions
- Breaks or interruptions in thought leading to incoherence, irrelevant speech, or neologisms
- Catatonic behavior
- Negative symptoms
- Significant changes in overall behavior, such as loss of interest and social withdrawal
In contrast to the DSM-5-TR, the ICD-10 categorizes schizophrenia based on key presenting symptoms into various types, including:
- Paranoid schizophrenia
- Hebephrenic schizophrenia
- Catatonic schizophrenia
- Undifferentiated schizophrenia
- Post-schizophrenic depression
- Residual schizophrenia
- Simple schizophrenia
- Schizophrenia, other
- Schizophrenia, unspecified
Evaluation of Schizophrenia
Schizophrenia is primarily a Clinical diagnosis, but specific radiographic and laboratory tests are necessary to rule out other potential causes. The American Psychiatric Association Practice Guideline for the Treatment of Patients with Schizophrenia recommends the following evaluations during an initial assessment:
1. Hematology
A complete blood count (CBC) should be performed to check for anemia or signs of infection that may mimic schizophrenia symptoms. If the patient is being considered for treatment with clozapine, an absolute neutrophil count (ANC) should also be obtained.
2. Blood Chemistry Panel
This should include tests for electrolytes, renal function, liver function, and thyroid-stimulating hormone (TSH). Hypothyroidism can present with psychiatric symptoms such as depression and cognitive impairment.
3. Pregnancy Test
A pregnancy test is recommended for women of childbearing age.
4. Electroencephalogram (EEG)
An EEG may be warranted based on the neurological examination or patient medical history to rule out seizure disorders.
5. Imaging
Brain imaging tests, either a CT or MRI (with MRI being preferred), may be indicated based on neurological findings or patient medical history.
6. Genetic Testing
Chromosomal testing is suggested if indicated by the physical examination or developmental clinical history.
7. Drug Toxicology Screen
This screen may be necessary to identify substance use that could lead to psychotic symptoms.
Treatment of Schizophrenia
The treatment of schizophrenia typically involves a comprehensive approach that combines medication, psychotherapy, and supportive services. Here are the key components:
1. Medications
- Antipsychotics: These are the cornerstone of schizophrenia treatment. They can help manage symptoms such as delusions, hallucinations, and disorganized thinking. There are two main categories:
- Typical (First-Generation) Antipsychotics: Examples include haloperidol and chlorpromazine. These primarily target dopamine receptors but may have more side effects, such as extrapyramidal symptoms.
- Atypical (Second-Generation) Antipsychotics: Examples include risperidone, olanzapine, and aripiprazole. These tend to have a lower risk of motor side effects and can also address negative symptoms.
2. Psychotherapy
- Cognitive Behavioral Therapy (CBT): This can help patients manage symptoms and improve functioning by challenging distorted thoughts and developing coping strategies.
- Supportive Therapy: Providing emotional support, practical assistance, and education about the mental disorders can be beneficial.
- Family Therapy: Involving family members can enhance support and improve communication.
3. Rehabilitation and Support Services
- Psychosocial Rehabilitation: Programs focused on social skills training, vocational rehabilitation, and community support can help individuals reintegrate into society and improve quality of life.
- Case Management: Coordinated care by case managers can assist patients in accessing services and navigating the healthcare system.

.jpg)
NEET-PG 2024 was conducted on 11th August,2024 in two shifts for admission to MD/MS/DNB/Diploma Courses of 2024-25 admission session.
The result of NEET PG 2024 has been declared and can be seen at NBEMS websites: https://natboard.edu.in/viewNotice.php?NBE=WFVQMUZiVWVUWkhwUlZoYXR3TjhZdz09
In accordance with the minimum qualifying/eligibility criteria for admission to MD/MS/DNB/Diploma Courses as mentioned in the Information Bulletin for NEET PG 2024, the cut-off percentile for various categories are as follows:
| Category | Minimum Qualification/Eligibility Criteria |
| General / EWS | 50th Percentile |
| General-PwBD | 45th Percentile |
| SC/ST/ OBC (Including PwBD of SC/ST/OBC) | 40th Percentile |
The merit position for All India 50% quota seats shall be declared separately. The final merit list/category wise merit list for State quota seats shall be generated by the States/UT as per their qualifying/eligibility criteria, applicable guidelines/regulations & reservation policy.
Individual scorecard of the candidates who appeared in NEET-PG 2024 can be downloaded from the website https://nbe.edu.in/ on after 30th August 2024.
Candidature is purely provisional subject to fulfillment of eligibility criteria as mentioned in the NEET-PG 2024 Information Bulletin and verification of their Face ID/Biometric wherever required.